Breast Cancer Connect recently hosted a discussion with Medical Oncologists regarding the treatment of Early Breast Cancer (EBC).
Below are some highlights from the discussion:
Responding oncologists initially perform a detailed review including pathology/medical review, imaging, bone density, cancer staging, and Oncotype DX. Oncologists focus on the need for chemotherapy.
- “[I consider] detailed pathology review, oncotype testing, comorbidities, bone density status, and contraindications to endocrine therapy.”
- “Initially, I rely on my colleagues in radiology to help guide diagnostic mammograms, US, and MRI as necessary. This is followed by appropriate biopsy. Then, we rely on pathology to provide us with diagnostic information including ER/PR/HER2 and Ki67 status. Once we have diagnostic and pathologic information, we can then decide on a treatment approach most appropriate.”
- “I typically look at the staging and the pathology. We look at the receptor status. We also do oncotype Dx to decide on further management.”
Treatment is facilitated by specialty breast cancer clinics.
- "At a community setting, something hard to get pathology, radiology, surgery, med onc, rad onc all on board. Unfortunately, we do not have one clear ‘breast cancer clinic.’ So, it does end up being a number of visits for patients.”
- “Actually, not too many challenges. We have a good breast center with excellent breast radiologists, good equipment, too, with MRI, etc. Also, excellent surgeons … so if we have a good biopsy and the path is read out, we will have a good plan. We also have a weekly multidisciplinary team conference."
Oncologists tend to educate patients without the use of too many outside sources but find the NCCN guidelines and Oncotype DX score report useful.
- “I try to estimate risk of recurrence and estimate the benefit of therapy in lowering the risk. The Oncotype DX score report is very helpful. I also I review the NCCN guidelines with the patient.”
- “I spend the first hour to two hours at the initial visit educating the patient about the findings on mammogram, breast MRI, path report, overview of endocrine therapy and chemotherapy, review of regimen and their side effects. Once we settle on specific one, my nurse practitioner has a 45-minute chemo teaching session or 30 minute targeted therapy teaching session.”
Respondents didn’t think that PD-1 inhibitors are effective in HR+ disease.
- “I think the jury is still out on how they will play a role for ER+/HER2-negative patients. I hope we can see them studied in late phase clinical trials and hopefully will show some benefit. Unfortunately, I just don't think we are quite there yet with the available data that we have.”
- “Not aware of any data proving their utility in ER-positive disease.”
- “Doubt that there will be any role in the early stage, only in high CPS [combined positive score].”
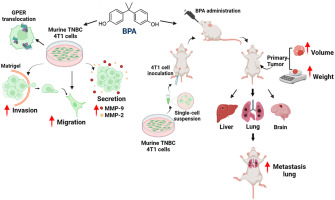
Respondents stated that the benefit of PD-1 inhibitors is for patients with triple-negative breast cancer.
- “I am not very optimistic about PD-1 inhibitor in EBC, ER+/HER2- BC. The benefit data is mainly in the triple-negative breast cancer category.”
- “I am not sure. It is only looked at now in the TNBC as in Keynote 522, but I know trials are underway. We shall see soon.”
Estimates for local recurrence were about 10%, with estimates on distance recurrence ranging more widely.
- "Small numbers, perhaps under 10% have local relapse and less than 3-4% with distant.”
- “Hard to answer in abstract, different patients have different risks. I estimate that 10% will have local recurrence and 25% distant recurrence.”
- “Local relapse is 10%, and late relapse is 15%.”
- “Depends on whether you are considering stage I of stage I + II early stage. I would guestimate a risk as high as 6% of local recurrence and lifetime risk between 19% and 30% of distant relapse, which varies according to whether they received adjuvant regimen.”
Lumpectomy vs. mastectomy plays a role.
- “It depends on whether or not they have a lumpectomy or mastectomy. Risk of post mastectomy local recurrent is quite low. If patient has had a lumpectomy, if they receive radiation the risk is slightly higher, but overall, still less than 10%. Risk of distant relapse is between 10-15%.”
Oncologists were interested reviewing longer-term data regarding CDK 4/6 inhibitors in the adjuvant setting, as well as data in the neoadjuvant setting.
-
 Ali Mirmiran2yrI would also take into consideration size of tumor to breast size ratio.
Ali Mirmiran2yrI would also take into consideration size of tumor to breast size ratio. -
 Albert Dekker2yrit is also depends on size of breast, chest wall, potential for reconstruction and other factors; if mastectomy is performed; bilateral mastectomy should be always considered
Albert Dekker2yrit is also depends on size of breast, chest wall, potential for reconstruction and other factors; if mastectomy is performed; bilateral mastectomy should be always considered